IgE-mediated hypersensitivity
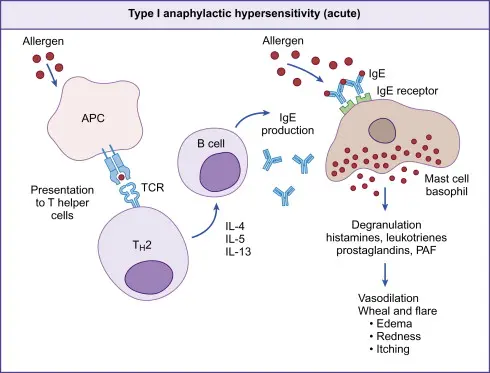
IgE-mediated hypersensitivity, known as type I or immediate hypersensitivity, involves an exaggerated immune response where allergen-specific IgE antibodies trigger mast cell and basophil degranulation upon re-exposure to allergens.
Mechanism
In IgE-mediated (type I) hypersensitivity, an allergen is first taken up by an antigen-presenting cell (APC), processed, and presented on MHC class II to a naïve T helper cell, which differentiates into a Th2 cell. The Th2 cell secretes cytokines such as IL-4, IL-5, and IL-13 that stimulate B cells to undergo class switching and produce allergen-specific IgE antibodies. These IgE molecules bind to high‑affinity FcεRI receptors on the surface of mast cells and basophils, arming them for future reactions. Upon re-exposure, the same allergen cross‑links the IgE on these cells, triggering degranulation and release of mediators including histamine, leukotrienes, prostaglandins, and platelet-activating factor, which cause vasodilation and increased vascular permeability, clinically manifesting as wheal and flare, edema, redness, and itching.
Clinical Manifestations
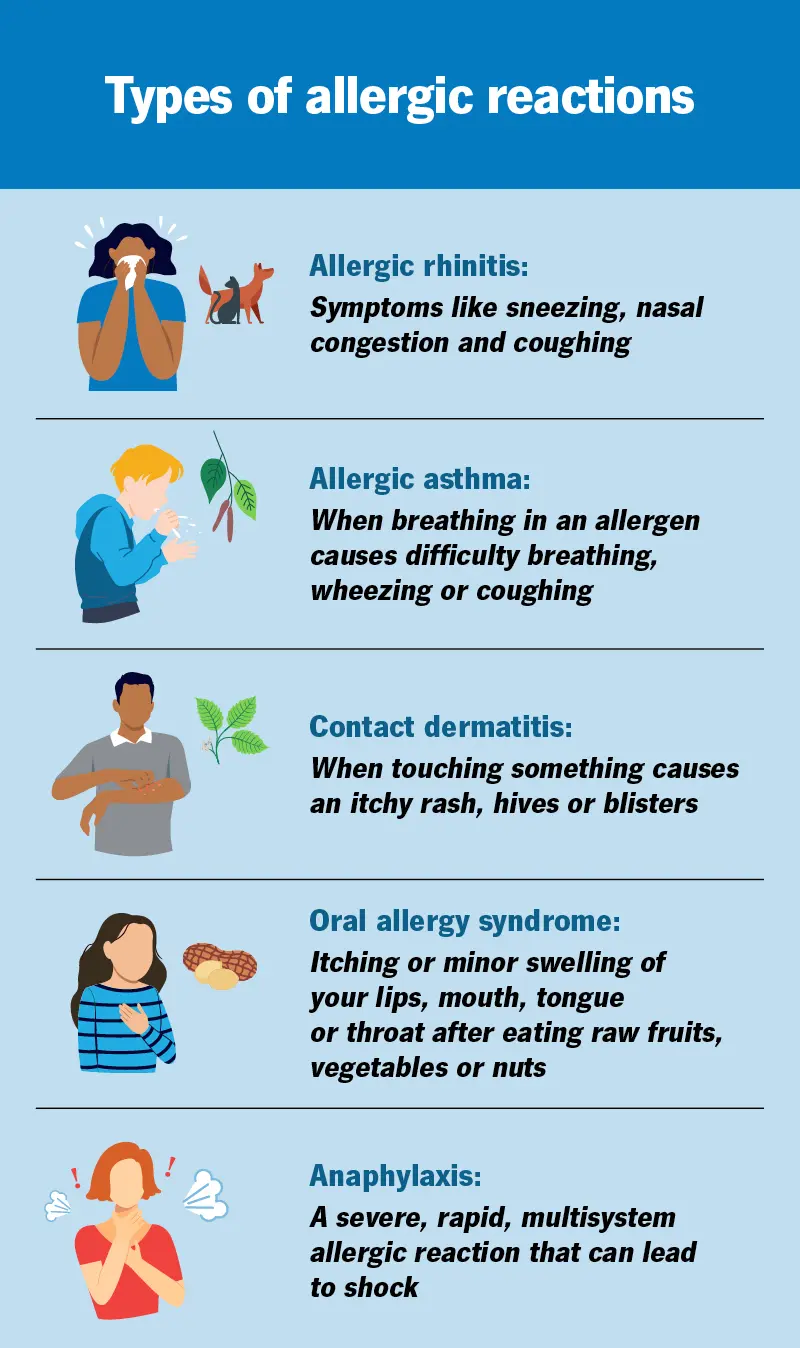
Allergic reactions can appear as hives, allergic rhinitis, asthma, eczema, food allergies, or severe reactions such as anaphylaxis. These responses may involve ongoing inflammation in the body. Allergies affect nearly one-third of the global population and are commonly triggered by environmental allergens such as pollen, dust mites, certain foods, and insect venom.